What Is Gastroshiza?
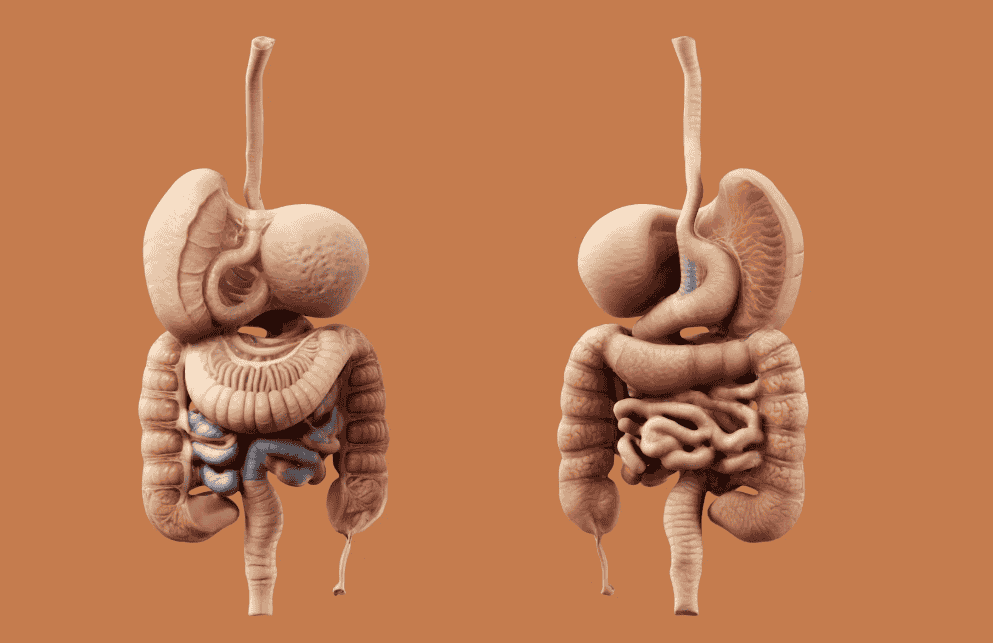
Gastroshiza, also known as gastroschisis, is a birth defect that affects the abdominal wall. It occurs when a baby is born with their intestines or other abdominal organs outside their body, protruding through a hole near the belly button. Unlike other congenital conditions, gastroshiza is not enclosed by a membrane, leaving the organs exposed. Understanding the causes, treatment options, and outcomes can provide clarity for those affected by or interested in this condition.
The exact cause of gastroshiza remains unclear, but it is believed to result from improper development of the baby’s abdominal wall during early pregnancy. Although rare, the condition has become slightly more common in recent decades. With modern medical care, however, most infants with gastroshiza can recover and thrive. By examining symptoms, management, and outcomes, this article aims to shed light on gastroshiza to help families and individuals understand what to expect.
Causes and Risk Factors for Gastroshiza
The development of gastroshiza is complex, with no definitive explanation for its occurrence. However, several risk factors are commonly associated with the condition:
- Age of mother: Younger mothers under 20 are at higher risk of giving birth to babies with gastroshiza.
- Lifestyle factors: Smoking, alcohol use, or drug consumption during pregnancy can increase the likelihood.
- Low socioeconomic status: Limited access to proper prenatal care is another contributing factor.
Family history of the condition does not appear to be a significant risk, which suggests gastroshiza is not strongly linked to genetic factors. Some studies propose that environmental influences during pregnancy, such as exposure to pesticides, might play a role.
While more research is needed to fully understand gastroshiza’s causes, recognizing potential risk factors can help expectant mothers focus on preventive measures, like eliminating harmful substances and accessing regular prenatal care.
Recognizing Gastroshiza During Pregnancy
Gastroshiza is typically detected through routine prenatal tests. The most common methods include:
- Ultrasound: An anomaly scan conducted between 18 and 22 weeks of pregnancy can usually identify the defect.
- Maternal serum screening: Higher levels of alpha-fetoprotein (AFP) in the mother’s blood can indicate abdominal wall defects like gastroshiza.
Early detection allows doctors to plan for specialized care, which is crucial for the baby’s survival and recovery. Mothers carrying a baby with gastroshiza will likely require more frequent monitoring, including ultrasounds and consultations with specialists.
The presence of gastroshiza can be alarming for parents, but early diagnosis offers a better chance to address potential complications and optimize outcomes for the baby.
Treatment Options for Gastroshiza
Surgical intervention is necessary to treat gastroshiza. The primary goal is to protect the exposed organs and place them back inside the baby’s abdomen. Treatment generally involves:
- Staged repair:
- For babies with large defects, a silo bag is positioned over the protruding organs immediately after birth to protect them. The organs are then gradually reintroduced into the abdomen over several days.
- Immediate closure:
- For smaller defects, surgery is performed shortly after birth to close the hole and reposition the organs.
Advances in neonatal care mean most babies with gastroshiza receive treatment within their first week of life. Post-surgery, infants may remain in the neonatal intensive care unit (NICU) for a few weeks to ensure proper organ function and recovery.
Possible Complications and Long-Term Outlook
While gastroshiza is treatable, some complications may arise. These include:
- Digestive issues: Babies might initially struggle with feeding or absorption due to underdeveloped intestines.
- Growth delays: Some children experience slower growth trajectories, though this typically resolves over time.
- Short bowel syndrome: Rarely, parts of the intestine may require removal, impacting nutrient absorption.
The long-term outlook for children with gastroshiza is overwhelmingly positive. With proper medical care and monitoring, most individuals go on to lead normal, healthy lives. Regular follow-ups with pediatric specialists can help address any lingering digestive or nutritional concerns.
Preventive Measures During Pregnancy
While not all cases of gastroshiza can be prevented, there are certain steps expectant mothers can take to reduce risk:
- Avoid smoking, alcohol, and drugs entirely during pregnancy.
- Maintain a nutritious diet rich in folic acid and essential vitamins.
- Schedule regular prenatal checkups to monitor your baby’s development.
Creating a healthy environment during pregnancy plays a significant role in minimizing risks, not only for gastroshiza but for various other complications.
Support and Resources for Families
Navigating a diagnosis of gastroshiza can be emotionally overwhelming for families. Fortunately, there are numerous support systems available, including:
- Healthcare providers who specialize in fetal medicine and neonatal care.
- Support groups for families facing similar outcomes, offering emotional guidance and shared experiences.
- Online communities, blogs, and forums where people share advice and information about gastroshiza care.
Seeking help early and connecting with others in similar situations can make a huge difference in coping with the condition.
Myths and Misconceptions About Gastroshiza
Despite medical advancements, many myths about gastroshiza persist. Some common misconceptions include:
- “It’s the parents’ fault.” Gastroshiza has no single cause and isn’t directly the result of actions or inactions during pregnancy.
- “It runs in families.” This is untrue; gastroshiza is rarely linked to family medical history.
- “Babies with gastroshiza cannot thrive.” With proper care, most children with this defect go on to live healthy, active lives.
Providing accurate information is essential in combating such myths and supporting affected families.
Advances in Research and Future Prospects
Medical research continues to improve outcomes for babies born with gastroshiza. Innovations in surgical techniques and neonatal care have significantly reduced complications. Studies are also exploring the roles of environmental exposures and maternal health factors to better understand the condition. With continued research, we may soon uncover more effective ways to prevent and treat gastroshiza.
FAQs About Gastroshiza
What causes gastroshiza?
The exact cause is unknown, though risk factors include maternal age under 20, smoking, and environmental exposures. It’s not typically hereditary.
Can gastroshiza be detected before birth?
Yes, it’s often identified through ultrasound and maternal serum screening during routine prenatal care.
What are the treatment options for gastroshiza?
Treatment involves surgery to reposition the exposed organs and close the abdominal wall. This may occur in stages or through immediate repair, depending on the defect’s size.
Are there complications after surgery?
Some babies experience digestive issues or short bowel syndrome, but most recover well with proper medical care and monitoring.
Can gastroshiza be prevented?
While not entirely preventable, avoiding harmful substances during pregnancy and receiving regular prenatal care can reduce risks.
Is gastroshiza life-threatening for babies?
Without treatment, gastroshiza can lead to serious complications. Fortunately, with modern medical advances, survival rates are high.
How long do babies stay in the hospital after surgery?
Most newborns with gastroshiza stay in the NICU for several weeks while their intestines adjust and start functioning properly.
Will a baby with gastroshiza have a normal life?
Yes, most individuals with gastroshiza go on to live healthy, normal lives with no major restrictions after recovery.
Are there organizations that support families dealing with gastroshiza?
Yes, many nonprofits, online groups, and hospital programs provide resources and emotional support for affected families.
Conclusion
Gastroshiza may be a challenging diagnosis, but understanding the condition is the first step toward managing it effectively. From early detection and advanced surgical options to comprehensive postnatal care, medical science provides a clear path forward for affected infants and families. Regular prenatal monitoring and a healthy lifestyle during pregnancy can significantly reduce risks and improve outcomes. With proper care and support, children born with gastroshiza can thrive and live fulfilling lives. Use available resources and connect with support groups to ease your journey and help your little one flourish.